Like every other insurance plan out there (auto, homeowners, disability), there is no “one size fits all” model. Instead, the differences lie in the size of the premiums, and how restrictive the plan is with regards to the consumer’s choice of doctor.
Medical insurance is broadly distinguished as being basic insurance or major medical. A person may not know what their plan falls under. Most likely you are more familiar with the medical insurance terms HMOs, PPOs, high-deductible plans, Medicare and Medicaid. Looking more closely at what these medical insurance options are will assist you with becoming a more informed consumer.
Basic Health Insurance:
Basic health insurance is minimum essential coverage (MEC) that cannot exclude pre-existing conditions. Obama’s 2010 Affordable Care Act (ACA) made MEC required by law to be included in all health insurance plans. And although tax payers will no longer be penalized financially for not carrying health insurance meeting MEC standards, insurance carriers are still mandated to adhere to offering MEC in every plan sold.
But what is minimum essential coverage (MEC)
Per ACA, all health insurance plans sold today are required to offer 10 categories of basic medical services. These services are:
- Emergency services
- Physician wellness visits and chronic disease management
- Pregnancy and childbirth
- Hospitalization
- Outpatient hospital care
- Prescription drugs
- Laboratory services
- Pediatric care
- Rehabilitative services and devices
- Mental health/substance abuse services.
Although basic health coverage is overseen federally by regulations and standards, the insurance plans are privately purchased by consumers and are not subsidized government programs, such as Medicare and Medicaid.
Major Medical Insurance:
Major Medical coverage encompasses those programs people hear most often and are Health Maintenance Organizations (HMOs), Preferred Provider Organizations (PPOs), and High-Deductible Health Plans (HDHPs). Most people recognize the plan acronyms, but may not really know what these entail.
Health Maintenance Organizations (HMOs):
HMO plans offer a multitude of healthcare services through a network of providers who agree to supply an array of services to members. With an HMO you choose a primary care physician (PCP) who is your point of contact to obtain referrals to specialists on an as needed basis. You won’t be covered in the event you see a physician out of network or without a referral from your PCP.
Preferred Provider Organizations (PPOs):
A PPO is described as a type of managed care health insurance plan that provides maximum benefits if you visit an in-network physician or provider, but will still cover some of the cost if you visit out-of-network providers. You will not need a referral to see any physician or specialist, however, you may pay more out of pocket if that doctor is not within your network. To learn more about this, read our article The Tangled Webs Behind PPO Insurance Networks.
High-Deductible Health Plans (HDHPs):
High deductible plans can look appealing to consumers because of their low premiums. However, the trade-off is in high deductibles, that can be in the thousands for even individuals. An added feature of these plans is the option to open a Health Savings Account (HSA). HSAs are a type of savings account, which is debited with pre-tax money from your paycheck, much in the same way as your 401K.
The intended purpose of HSA contributions is to pay for medical expenses you incur and have to pay for since your high deductible has not been met. This being said, there are restrictions on how you can use the funds in an HSA. Some examples of qualified medical expenses are acupuncture, chiropractor, therapy, special education, hearing aids, medicines and eye glasses. Any unused funds in your account roll over automatically each year and remain indefinitely until used. There is typically no time limit on using the funds. The IRS does restrict the amount of money you can contribute to your HSA each year and the amount is updated annually due to inflation.
Does your health insurance plan qualify as a HDHP?
For 2019, the IRS has directed that any health insurance plan with a minimum annual deductible of $1,350 for an individual, or $2,700 for a family, constitutes being an HDHP. If you want to find out more information on opening an HSA, you can read more online at HSACenter.com.
Medicaid:
Medicaid is a federally funded subsidy that is offered to low-income individuals or those with disabilities, either for free or at a low-cost. Many states, like Illinois, expanded their Medicaid programs to coverage all people below poverty level. In Illinois, that income level is about $15,860 for an individual, or $32,500 for a family of four. (“Medicaid coverage to expand in Illinois” Chicago Tribune July 23, 2013 by Peter Frost and Rick Pearson)
“Obamacare”/The Affordable Care Act (ACA):
Illinois has a partnership with the federal government to offer coverage under the ACA through the health insurance exchange, accessible at HealthCare.gov. It’s important to distinguish that All Obamacare health insurance plans are “major medical” health insurance plans. That means they’re traditional health insurance plans that are designed to cover both minor and major medical issues.
Medicare:
Medicare is a federal health subsidized program that extends health coverage for people age 65 or older, those younger than 65 with certain disabilities, and people with End-Stage Renal Disease (ESRD), which is permanent kidney failure requiring dialysis or a transplant to survive. Medicare Part A coverage reimburses for inpatient hospital care and Part B is for doctor visits and outpatient care. Prescription drug coverage is not automatically included and can be added to your Medicare Part A and B for an additional cost.
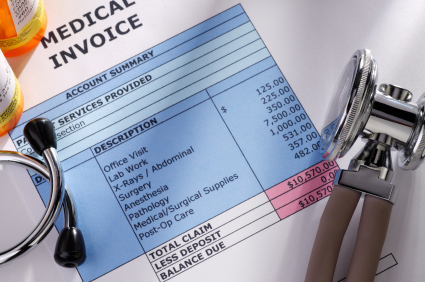
Accident Insurance:
A lesser known medical insurance plan is accident insurance which covers qualifying injuries, in which claim money can not only be used for medical bills but also mortgage payments or anything needing to be paid.
Critical Illness:
Critical illness insurance provides additional coverage after your primary medical insurance plan has been exhausted. It pays you if you’re diagnosed with a qualifying medical condition, such as Alzheimer’s disease, heart attack, paralysis, stroke or life-threatening cancer, to name a few. Claim money received on this plan can be used for any purpose, and not just to pay medical expenses.
This type of insurance is something you need to be accepted into and applications are underwritten much in the same way as life insurance. Therefore, acceptance into the plan is not guaranteed. Carriers decide whether or not to accept the risk of insuring you. Critical illness coverage is fairly new and was first widely marketed in the late 1990s to assist those people overrun with medical bills due to serious illness or injury afflictions.
The earliest version of this type of coverage was first seen in 1983 in Africa and called Dread Disease Insurance. Since the late 1990s, it’s found its way into the mainstream marketplace and is available by carriers such as Liberty Mutual, Aflac, Mutual of Omaha and Assurity.
Travel insurance also has medical payment coverage in case you are injured or ill while on vacation. It is purchased on a temporary basis and not kept year-round.